Lecture Series on Dental Caries
To watch video lectures, click at the following links
1. Introduction
3. Bacterial plaque in dental caries
4. Microbiology of dental caries
6. Acid production in dental plaque
A coaching institution for ADC examination, and Government dental jobs exam.
To watch video lectures, click at the following links
1. Introduction
3. Bacterial plaque in dental caries
4. Microbiology of dental caries
6. Acid production in dental plaque
In this chapter, you will know about the treatment planning of dental caries. In previous chapter you studies the etio-pathogenesis and clinical characteristics of dental caries. If you have not gone through it, it is advised that you study the previous chapter before proceeding further.
When the oral environment of a person is favourable where the pH is above 5.5 and saliva contains enough calcium and phosphate ions, the remineralisation process of enamel occurs. The supersaturated saliva acts as driving force for remineralisation. In a non cavitated enamel caries lesion, the original crystalline structure of rods remains intact. When it is etched, it acts as nucleating agent for remineralisation. When trace amount of fluoride ions is added to the environment, it enhances the remineralisation process by enhancing the precipitation of calcium and phosphate. The inclusion of fluoride ions results in the formation of fluorapatite crystals in enamel rods which is more resistant to acid attack compared to calcium apatite of the natural enamel rods. Thus, the new enamel becomes resistant to caries process.
This lesson presents basic definitions, terminologies, etiologies, demineralisation-remineralisation of enamel and clinical characteristics of the caries lesion in the context of clinical operative dentistry.
Dental caries is defined as a multifactorial, transmissible, infectious oral disease caused primarily by the complex interaction of cariogenic oral flora (biofilm) with fermentable dietary carbohydrates on the tooth surface over time.
Dental plaque is a gelatinous mass of bacteria adhering to the tooth surface. Carious lesions occur only under the plaque. The plaque bacteria metabolises the refined carbohydrate (sucrose mainly) for energy production and produces organic acids as a by product. These acids cause dissolution of crystalline structures of enamel that result in caries lesions of the tooth.
Hepatitis is an inflammation of the liver that's caused by a variety of contagious viruses and non-infectious agents leading to a range of health problems, some of which can be fatal. There are five main strains of the hepatitis virus, known as types A, B, C, D and E. While their infection results in liver disease, they differ in important ways including modes of transmission, severity of the illness, geographical distribution and prevention methods.
In this first part of the article, we shall discuss the following aspects of hepatitis:
Hepatitis B is a potentially life-threatening liver infection caused by the hepatitis B virus (HBV). It can cause chronic infection and puts people at high risk of death from cirrhosis and liver cancer.
In the first part of the article, you have read the epidemiology, mode of transmission of Hepatitis B virus, its sign and symptoms, groups at risk, the relationship of HBV and HIV infection, and how the diagnosis is confirmed. In this part of the article, we shall discuss about its treatment and prevention.
If you want to read a short note on Hepatitis B in Indian context, read it HERE.
You can also take a free mock test on Hepatitis B.
Dental caries is an endemic disease in children. It is caused by a bacterial infection. The causative bacteria are known as Streptococcus Mutans and Lactobacilli.
Although the dental caries is caused by bacteria, the initiation and progression of dental caries depend on several factors. The less the risk factors present, the less are the chances of dental caries development in your child’s tooth.
I shall discuss those factors for you so that you can understand the developmental process of dental caries and take appropriate measures to prevent developing it in your son’s or daughter’s mouth. Broadly, we can categorize a child belonging to either high risk or low risk category. The children of high-risk category have higher chances of developing dental caries compared to those of lower category.
The factors that determine the risk category of a person are as follows:
So, now you know the causes that may put your child at high risk for developing dental caries. I advise you to understand these factors and take appropriate action. The first step you must take is to start using a toothpaste that contains either fluoride or CCA-ACP. Also, plan for and have your child get checked by a dentist.
The quality of dental treatment of a child depends on one's cooperation and repo with a dentist in the treatment room. How a dentist manages a child depending upon the understanding the child's behaviour pattern.
There are certain guidelines that are useful in helping a child to show a positive & compliant behaviour while getting the dental treatment. These guidelines have been prepared from the findings and principles of behavioural dentistry, behavioural psychology, developmental psychology, and paediatric psychology.
The
alginate impression material cannot be used as muco-compressive material. This
material does not have consistency enough to apply pressure on mucosa.
Therefore, muco-compressive impressions cannot be taken by alginate.
The muco-compressive impression can only be taken by impression compound or heavy duty (putty) rubber base impression materials as they both have thick consistency.
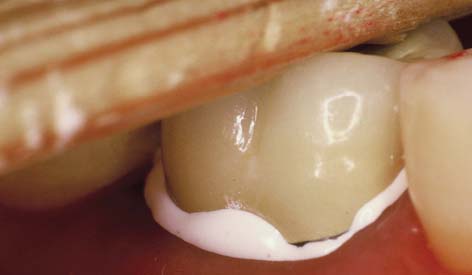
The placement of crown is an important step in the longevity of the crown and the comfort of the patient. There are certain points that should be taken into consideration by a dentist during placement i.e. cementation.
The gingival margins should not be inflamed at the time of crown cementation. This may happen due to gingivoplasty or crown lengthening. For a common man, it means, the gum margins of the tooth receiving the artificial crown should not have redness, swelling or puffiness. If there is any, better to wait till it subsides.
The choice of cement/luting agent should be decided based on the type and material of the crown. The available materials are Zinc phosphate, Glass ionomer, Polycarbonate, Zinc silicophosphate, and resin luting agents. The anterior crowns need different cementing material than that of posterior crowns. The all ceramic crowns are best cemented by resin luting agents, but the use is limited to the cementation of anterior crowns. The reason is, after cementation, it becomes extremely difficult to remove set resin from the interproximal area of posterior teeth. Rest luting materials are brittle enough to break and remove, therefore, they can be used in all areas-anterior as well as posterior.