Oral candidiasis is a fungal disease that is caused by Candida albicans. It looks like a white or creamy plaque or patch that can be wiped off with the help of a cotton swab or a tooth brush leaving a red base.
 |
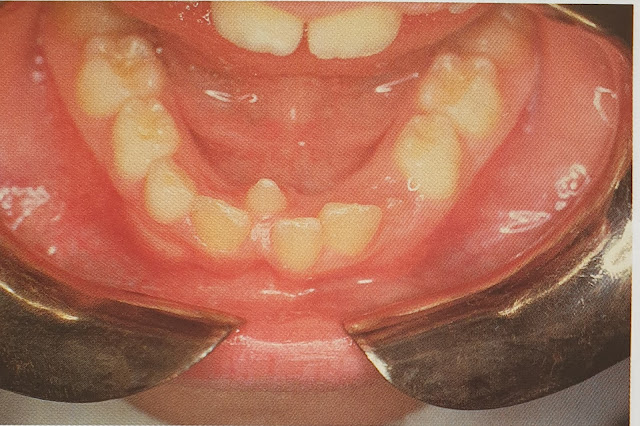
| Gingival thrush |
It occurs due to disturbance in the oral microflora due to antibiotics, corticosteroid, Xerostomia , immune defects especially in HIV infection, immunosuppressant, leukaemia or lymphomas and diabetes. It rarely occurs in a healthy individuals except in neonates.
 |
| Chronic mucocutaneous candidosis: note the wide adherent plaque. |
Gram stain smear shows the Candida albicans hyphae. It should be differentiated from Koplik's spot or Fordyce's granules.
The treatment involves treating the cause. Antifungal agents, for example, nystatin oral suspension or pastilles, amphotericin lozenges, or miconazole gel or tablets or fluconazole tablets can be given.
Ref:
1. Oral diseases 2nd Ed. Crispian Scully, Roderick A. Cawson Churchill Livingstone